Osteoarthritis of the hip is a degenerative-dystrophic disease characterized by destruction of hyalinized cartilage.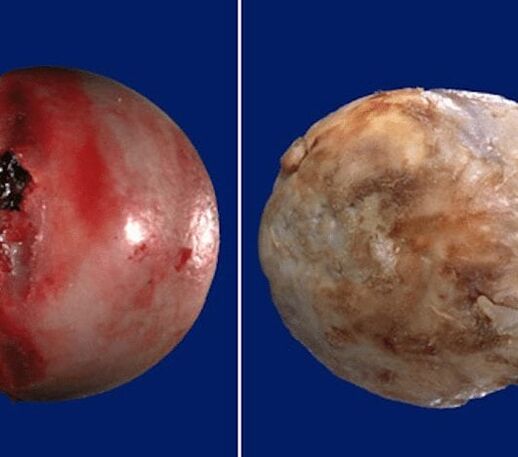 The disease develops gradually, accompanied by pain and reduced range of motion. In the absence of medical intervention in the early stages of joint disease, after a few years, femoral muscle atrophy occurs.
The disease develops gradually, accompanied by pain and reduced range of motion. In the absence of medical intervention in the early stages of joint disease, after a few years, femoral muscle atrophy occurs. The injured limb is shortened, and the fusion of the joint space leads to partial or complete immobilization of the hip. The cause of the pathology is due to previous trauma, curvature of the spine, systemic diseases of the musculoskeletal system.
The injured limb is shortened, and the fusion of the joint space leads to partial or complete immobilization of the hip. The cause of the pathology is due to previous trauma, curvature of the spine, systemic diseases of the musculoskeletal system.
Osteoarthritis is usually detected in middle-aged and elderly patients. Diagnosis is made on the basis of the results of instrumental studies - radiography, MRI, CT, arthroscopy. Treatment of grade 1 and grade 2 pathology is conservative. If ankle sprains are found or drug treatment is not effective, surgery (arthroscopic, arthroscopic) will be performed.
Mechanism of development of the disease
The hip joint is formed by two bones - the pelvis and the femur. The lower part of the ilium is represented by its body, which participates in the articulation of the femur, forming the upper part of the acetabulum. During movement, the sternum does not move and the femoral head moves freely. Such a "hinge" device of the hip allows it to flex, not bend, rotate, promoting abduction, complementation of the hip. Smooth, elastic, resilient hyaline cartilage surrounds the tibia and femoral head, allowing joint structure to slide unimpeded. Its main function is to redistribute the load during movement, preventing rapid wear of bone tissues.
Under the influence of external or internal factors, the vegetative process of cartilage is disturbed. It doesn't have its own circulatory system - synovial fluid supplies nutrients to tissues. With paresis, it thickens, becomes viscous.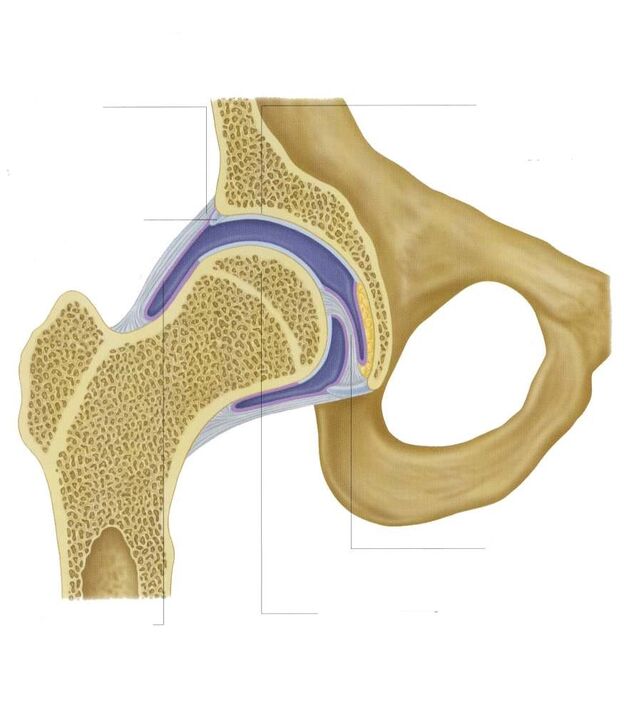 Nutrient deficiencies lead to dry surface of hyalinized cartilage. It is covered with fissures, resulting in permanent micro-damage during flexion or extension of the hip joint. Cartilage becomes thinner and loses its cushioning properties. Bones are deformed to "adapt" to the increase in pressure. And against the deterioration of metabolic processes in tissues, destructive and degenerative changes take place.
Nutrient deficiencies lead to dry surface of hyalinized cartilage. It is covered with fissures, resulting in permanent micro-damage during flexion or extension of the hip joint. Cartilage becomes thinner and loses its cushioning properties. Bones are deformed to "adapt" to the increase in pressure. And against the deterioration of metabolic processes in tissues, destructive and degenerative changes take place.
Causes and triggers
Idiopathic or primary joint disease that develops for no reason. It is believed that the destruction of cartilage tissue occurs as a result of the body's natural aging process, which slows down the recovery process, reducing the production of collagen and other compounds necessary for the full reconstruction of the joint structure. Crotch. Secondary arthropathy occurs against the background of an existing medical condition in the body. The most common causes of secondary disease include:
- previous trauma - damage to the ligamentous apparatus, muscle rupture, complete separation from the bone base, fracture, dislocation;
- violation of joint development, congenital dysplasia;
- autoimmune pathologies - rheumatic, reactive, psoriatic arthritis, systemic lupus erythematosus;
- nonspecific inflammatory diseases such as purulent arthritis;
- specific infections - gonorrhea, syphilis, brucellosis, ureaplasmosis, trichomoniasis, tuberculosis, osteomyelitis, encephalitis;
- disruption of the endocrine system;
- degenerative-dystrophic pathology - mastoid disease of the femoral head, osteomyelitis;
- increased mobility of joints, due to the production of "super-expanding" collagen, which stimulates their excessive mobility, weakens the ligaments.
Since the cause of the development of arthropathy can be hereditary (hemorrhage in the hip cavity), provoking factors include hematopoietic disorders. Prerequisites for the onset of the disease are overweight, excessive physical activity, sedentary lifestyle. Its development is due to improper organization of exercise, a diet lacking in foods rich in trace elements, fats and water-soluble vitamins. Postoperative fibrosis occurs several years after surgery, especially if it is accompanied by the removal of large amounts of tissue. The thermogenicity of hyaline cartilage causes discomfort with frequent hypothermia, living in an unfavorable environment and working with toxic substances.
Osteoarthritis of the hip cannot be inherited. But when there are certain innate features (metabolic disorders, bone structure), its growth potential increases significantly.
The symptoms
The leading symptom of hip osteoarthritis is pain when walking in the hip area, spreading to the hip and knee joints. A person has stiff movements, stiffness, especially in the morning. To stabilize the joint, the patient begins to limp, the gait changes. Over time, due to muscle atrophy and joint deformity, the limb shortens markedly. Another characteristic sign of pathology is limited hip flexion. For example, difficulty arises when trying to sit on a stool with two legs.

For first-degree arthropathy, periodic pain occurs after vigorous exertion. They are localized in the joint area and disappear after a long period of rest.
With second-degree arthritis of the hip joint, the severity of the pain syndrome increases. The discomfort occurs even at rest, extends to the thighs and groin, and increases with weight lifting or increased physical activity. To eliminate pain in the hip joint, a person begins to limp with a noticeable limp. Limited range of motion in the joint is noted, especially during flexion and internal rotation of the thigh.
Grade 3 arthritis is characterized by persistent, severe pain that does not subside day or night. Difficulty arises when moving, therefore, when walking, a person is forced to use a cane or crutches. The hip joint is stiff, there is atrophy of the buttocks, thighs, and legs. Due to the weakness of the thigh muscles, the pelvis is displaced in the anterior plane. To compensate for the shortened leg, the patient leans toward the injured limb when moving. This causes a drastic change in center of gravity and increases stress on the joints. At this stage of osteoarthritis, arthritis develops markedly.
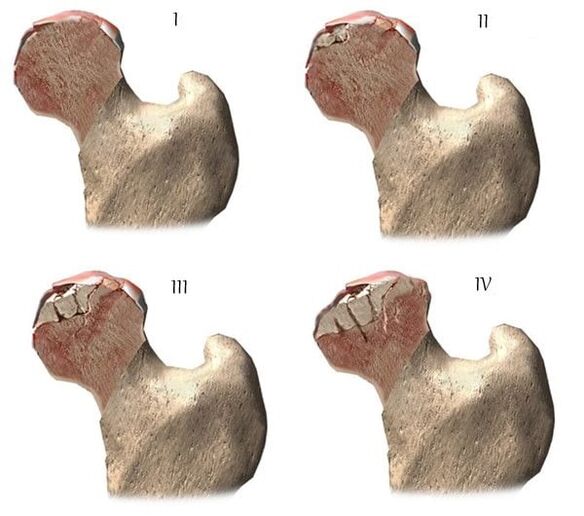
| Degree | Radiographic signs |
| The first | The changes are not obvious. The joint space is moderately narrow, irregular, with no superficial destruction of the femur. Small bony growths observed on the outer or inner edge of the mesh |
| Second letter | The height of the joint space is greatly reduced due to its uneven fusion. The femoral head is displaced upward, deformed, enlarged, uneven contours. Bone growth that forms on the surface of the inner and outer edges of the arachnoid bone |
| The third day | There is complete or partial fusion of the joint space. The femoral head is strongly extended. Many skeletons grow on all surfaces of the mesh |
Diagnose
When making a diagnosis, the doctor takes into account the clinical manifestations of the pathology, medical history, the results of the patient's external examination, and instrumental studies. X-rays are the most informative. With its help, the condition of the hip is evaluated, the stage of the course, the degree of damage to the cartilage tissues, and in some cases, the cause of the development is determined. If the cervical node is dilated, and the apex is oblique and flattened, there is a high probability that congenital dysplastic changes in the joint can be assumed. Perthes disease or juvenile poliomyelitis is manifested by the disordered shape of the hip bones. Radiographs can reveal post-traumatic joint status, even though there is no prior trauma during the history. Other diagnostic methods are also used:
- CT helps to detect the growth of the edges of the bone plates, the bone cells that have formed;
- MRI is performed to evaluate the condition of the connective tissue structures and the degree of their involvement in the pathological process.
If necessary, the inner surface of the joint is examined with arthroscopic instruments. Differential diagnosis is made to exclude gonadal cyst, lipoma, or thoracic osteoma. Pain in arthritis can be disguised as the clinical presentation of pinched or inflamed lenticular syndrome. Usually neuropathy can be ruled out with the help of a variety of tests. Osteoarthritis of the hip must be differentiated from hip bursitis, ankylosing spondylitis, and reactive arthritis. To exclude autoimmune pathologies, biochemical studies of blood and synovial fluid are performed.
Drug treatment strategies
Medical treatment is aimed at improving the patient's health. For this, drugs of different pharmacological and clinical groups are used:
- nonsteroidal anti-inflammatory drugs (NSAIDs)--Nimesulide, Ketoprofen, Diclofenac, Ibuprofen, Meloxicam, Indomethacin, Ketorolac. For acute pain relief, injectable solutions are used, and tablets, oral drugs, ointments, gels eliminate pain of mild or moderate severity;
- glucocorticosteroids - Triamcinolone, Dexamethasone, Hydrocortisone. They are used as intra-articular blockade in combination with local anesthetics Procaine, Lidocaine;
- muscle relaxants - Baclofen, Tizanidine. They are included in the treatment regimen for skeletal muscle spasms, compression of sensitive nerve endings;
- medicines that improve blood circulation in the joints - Nicotinic acid, Aminophylline, Pentoxifylline. Prescribed to patients to improve tissue performance, prevent disease progression;
- chondroprotectors. Only effective in stages 1 and 2 of rheumatic fever.
Rubbing ointments with a warming effect eliminates mild pain. The active components of external agents are capsaicin, cinquefoil, camphor, menthol. These substances are characterized by an analgesic, irritating, distracting effect on the spot. Compressed into joints with Dimethylsulfoxide, medical bile will help with puffiness, swollen thighs in the morning. Patients are recommended classical massage, acupressure or vacuum to treat coxarthrosis. Daily exercise therapy is an excellent prevention of further progression of joint disease.
Surgical intervention
With the ineffectiveness of conservative therapy or the diagnosis of a pathology complicated by ankylosing spondylitis, an operation is performed. It is not possible to restore cartilage tissue in joints damaged by osteoarthritis without prosthetic joint rehabilitation surgery, but with the right treatment, following all prescriptions, maintaining the right lifestyle, practicingBy performing therapeutic exercises, regular massage, taking vitamins and proper nutrition, you can prevent the process of damage and destruction of cartilage and hip joints.
























